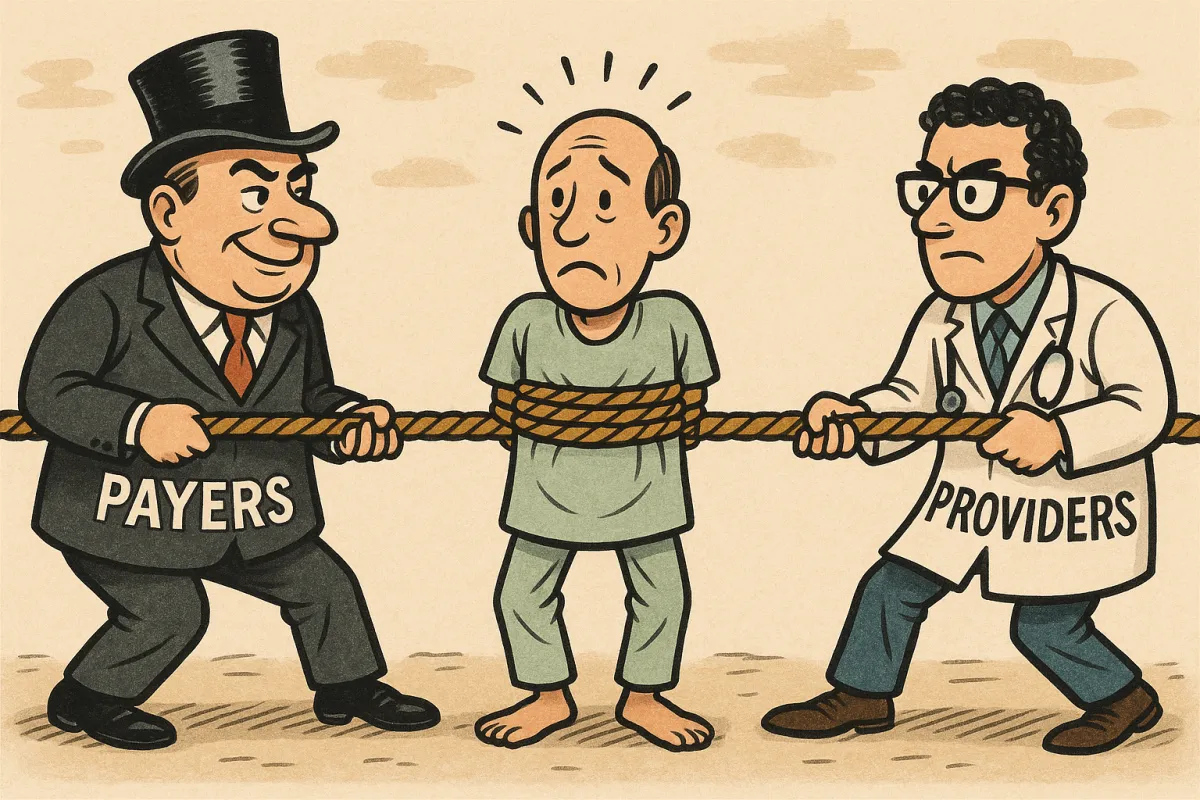
Who Pays the Price? The Patient in the Crosshairs of the Payer vs. Provider Battle
The recent news that UnitedHealthcare will drastically curtail coverage for Remote Patient Monitoring (RPM) across numerous chronic conditions starting in 2026 is a significant event. While framed as a simple business decision driven by a lack of "sufficient evidence of efficacy," this policy change is far more than an adjustment to billing codes. It's a stark indicator of a widening disconnect within the healthcare ecosystem.
The sentiment across the industry is that this move represents a major overshoot - a policy that prioritizes a narrow, short-term financial metric over the overwhelming evidence and strategic necessity of proactive care management.
The Misalignment Between Metrics and Value
It is true that payers are obligated to manage costs, and that poorly executed programs can fail to generate a measurable Return on Investment (ROI). This creates the grounds for insurers to tighten the eligibility reins.
However, denying coverage for established, high-incidence conditions such as Type 2 Diabetes and Chronic Hypertension departs from the contractual expectation that payers support reimbursement for clinically validated tools that enhance patient care and care continuity.:
Proactive Hypertension Management: Studies consistently affirm the effectiveness of remote oversight. For instance, a large, retrospective analysis linked RPM to significant reductions in blood pressure, with patients suffering from Stage 2 Hypertension seeing their Systolic Blood Pressure (SBP) improve by 16.7 mmHg after 90 days in a program [1].
Improving Diabetic Outcomes: Similarly, engagement in remote monitoring is associated with markedly better control, demonstrating a 23% higher likelihood of reaching target HbA1c goals in patients with newly diagnosed Type 2 diabetes [2].
This denial of proactive tools, despite strong clinical support, highlights a systemic problem: The system is punishing operational failure under the guise of insufficient clinical evidence.
The True Operational Challenge
The real barrier to sustainable value is not the concept of proactive monitoring itself - it is the difficulty of operationalizing excellence within existing clinic workflows.
When practices struggle to execute these programs, they often encounter:
Fragmented Workflows: Relying on manual processes and disparate technologies that lead to clinician burnout, alert fatigue, and errors.
Inaccurate Data: Inefficient management results in "dirty data" - information that is non-compliant, incomplete, and fails to demonstrate the consistent clinical value required to satisfy payer scrutiny.
When the operational infrastructure is flawed, the program's intended benefits - improved outcomes, reduced hospitalizations, and clear ROI - are lost. This operational gap is the vulnerability that policies like UHC's exploit, forcing providers to bear the burden of a system that rewards procedural compliance over clinical outcome.
Redefining Operational Integrity
Moving forward, success in the Fee-for-Service and Value-Based Care environments requires a relentless focus on operational integrity. It’s not enough to adopt technology; you must master the processes behind it.
Our focus is on helping organizations navigate this volatile landscape by ensuring their care management programs are built for both compliance and performance. We provide the strategic oversight and refined workflows that eliminate operational friction and transform raw data into a reliable clinical and financial asset. We are focused on value optimizing existing clinical services - providing the expertise needed to generate consistent, demonstrable results that withstand payer scrutiny and, most importantly, benefit the patient.
The future of healthcare depends on providers having the operational resilience to deliver high-value care, regardless of payer hurdles.
For more information or if you have any questions about optimizing your value-based care programs, feel free to reach out to us at [email protected].
Footnotes & Resources
[1] Source: Remote Patient Monitoring Is Associated with Improved Outcomes in Hypertension: A Large, Retrospective, Cohort Analysis.
URL: https://pmc.ncbi.nlm.nih.gov/articles/PMC11353537/
(Data point: SBP improved by 16.7 mmHg for Stage 2 HTN patients after 90+ days on an RPM program.)
[2] Source: UnitedHealthcare’s 2026 RPM Rollback: Why Limiting Remote Monitoring Hurts More Than It Helps.
(Data point: RPM participation linked to a 23% higher likelihood of reaching target HbA1c goals in patients with newly diagnosed Type 2 diabetes.)
[3] Source: Evidence and Recommendations on the Use of Telemedicine for the Management of Arterial Hypertension (American Heart Association Journals).
URL: https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.15873
(Data point: Telemonitoring plus active management resulted in greater reductions in BP, HbA1c, and a greater proportion of participants achieving their BP goal.)

